 In 1972 Liebow et al described a number of patients with a condition they called lymphomatoid granulomatosis (LYG) of the lung. Since then, other authors have described patients with this entity which is characterized by vasculitis with lymphoreticular infiltrate. Patients with this disease usually seek medical attention because of cough, excess sputum production, fever, dyspnea and weight loss. The pulmonary lesions tend to be in the lower lung fields, may be cavitary, and are generally unassociated with hilar lymphadenopathy. While most of the cases described in the literature have been treated with steroids alone or in combination with cytotoxic drugs, the efficacy of this treatment has not been established.
In 1972 Liebow et al described a number of patients with a condition they called lymphomatoid granulomatosis (LYG) of the lung. Since then, other authors have described patients with this entity which is characterized by vasculitis with lymphoreticular infiltrate. Patients with this disease usually seek medical attention because of cough, excess sputum production, fever, dyspnea and weight loss. The pulmonary lesions tend to be in the lower lung fields, may be cavitary, and are generally unassociated with hilar lymphadenopathy. While most of the cases described in the literature have been treated with steroids alone or in combination with cytotoxic drugs, the efficacy of this treatment has not been established.
We report a patient with LYG with impaired cell-mediated immunity. The patient has remained stable without specific treatment for the last eight years.
Case Report
A 65-year old woman was first admitted in 1975 with complaints of nausea, high fever, productive cough, breathlessness and chest pain. Her temperature was 40°C, the pulse rate was 1£0 beats per minute, and there were fine crepitant rales on both lung bases. Laboratory investigations at this time showed: Hb, 10.0 g%; WBC, 9,200 with a shift to the left; ESR, 80/110; albumin, 3.0 g; and globulin, 3.3 g; latex fixation test, 1:2,500-1:5,000; Rose Waaler, 1:64-1:128. Urine and blood cultures showed E coli and sputum cultures grew Klebsiella pneumoniae and Streptococcus viridans.
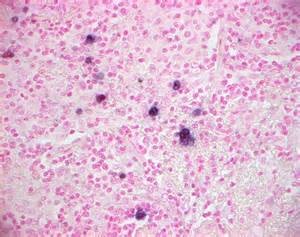
Chest x-ray films taken on admission revealed the presence of multiple round-shaped lesions in the left lower lobe and in the right middle and lower lobes (Fig 1). Radiographs of the sinuses, hand and spine were normal. Results of anti-DNA, ANF, LE cells, cryoglobulins, cold agglutinins, Weinberg- Casoni-Coombs test, and bone marrow aspiration were all negative. She was treated with gentamidn (Garamycin) and cephalexin (Keflex) and her condition improved gradually. A few weeks later she was readmitted with septic fever and this time sputum and blood cultures grew Diplococ-cus pneumoniae. She was again started on treatment with antibiotics, more information on Canadian Health&Care Mall (https://canadianhealthncaremall.com/what-antibiotics-could-help-for-cold.html) and the fever gradually abated. The findings of gross nodular lesions in both lung fields remained unchanged throughout both hospital courses. At this time, immunologic evaluation was performed.Serum immunoglobulins and complement levels were: IgG, 3,900 mg%; IgA, 330 mg%; IgM, 200 mg%; C3, 100 mg%; and C4 22.5 mg%. The number of peripheral blood T lymphocytes and immunoglobulins bearing В cells were normal flable 1). Results of delayed hypersensitivity skin tests to PPD, SK-SD and mumps vaccine were all negative. Dinitroclorobenzene (DNCB) skin sensitization was positive. The in vitro lymphocyte transformation with PHA was normal, while the transformation with Con-A and pockweed were significantly lower than in normal controls (Table 2). A percutaneous drill biopsy of the lung showed that the microscopic structure of the lung was totally obliterated by a dense, massive infiltration of lymphocytes, plasma cells and large hystiocytic-like cells dispersed between thickened collagen fibers (Fig 2). Occasional large, abnormal, hyperchromatic nuclei and a few mitotic figures were seen. Blood vessels showed thickening of the wall and occlusive changes (H and E stain, X100). These findings were consistent with the diagnosis of lymphomatoid granulomatosis.
Casoni-Coombs test, and bone marrow aspiration were all negative. She was treated with gentamidn (Garamycin) and cephalexin (Keflex) and her condition improved gradually. A few weeks later she was readmitted with septic fever and this time sputum and blood cultures grew Diplococ-cus pneumoniae. She was again started on treatment with antibiotics, more information on Canadian Health&Care Mall (https://canadianhealthncaremall.com/what-antibiotics-could-help-for-cold.html) and the fever gradually abated. The findings of gross nodular lesions in both lung fields remained unchanged throughout both hospital courses. At this time, immunologic evaluation was performed.Serum immunoglobulins and complement levels were: IgG, 3,900 mg%; IgA, 330 mg%; IgM, 200 mg%; C3, 100 mg%; and C4 22.5 mg%. The number of peripheral blood T lymphocytes and immunoglobulins bearing В cells were normal flable 1). Results of delayed hypersensitivity skin tests to PPD, SK-SD and mumps vaccine were all negative. Dinitroclorobenzene (DNCB) skin sensitization was positive. The in vitro lymphocyte transformation with PHA was normal, while the transformation with Con-A and pockweed were significantly lower than in normal controls (Table 2). A percutaneous drill biopsy of the lung showed that the microscopic structure of the lung was totally obliterated by a dense, massive infiltration of lymphocytes, plasma cells and large hystiocytic-like cells dispersed between thickened collagen fibers (Fig 2). Occasional large, abnormal, hyperchromatic nuclei and a few mitotic figures were seen. Blood vessels showed thickening of the wall and occlusive changes (H and E stain, X100). These findings were consistent with the diagnosis of lymphomatoid granulomatosis.
To improve the patients cellular immunity, levamisole was started at a dose of 50 mg three times a day, twice weekly. A week later, delayed hypersensitivity skin tests became positive; however, there was no improvement in the in vitro stimulation of lymphocytes by mitogens. Levamisole had to be stopped during the second week because the patient developed a severe hypersensitivity reaction.® The delayed hypersensitivity skin test became negative again, and there has been no improvement in the other immunologic parameters. Since then, and for the last eight years, the patients conditionhas remained stable without any specific treatment and x-ray films of the chest remained unchanged (Fig 1B).
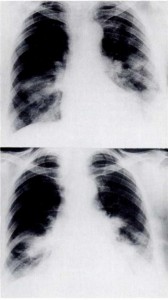
Figure 1A (upper). Bilateral lower lobe confluent nodular infiltrates present in both lung fields (April 20,1975). В (Lower). No significant change after six years (March 1,1981).
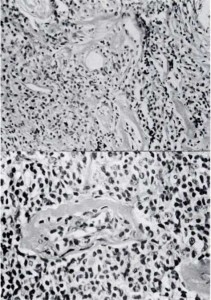
Figure 2A (upper). The microscopic structure is totally obliterated by a dense, massive infiltration of lymphocytes, plasma cells and large hystiocytic-like cells dispersed between thickened collagen fibers (Hematoxylin and eosin, original magnification x 30). 2B (lower). Higher magnification; note thickening of the wall and occlusive changes of the blood vessel (Hematoxylin and eosin, original magnification, x 100).
Table 1—Peripheral Blood Lymphoid Cell Markers
| % E Rosette (T cells) | % Ig + cells (B. Cells) IgG IgM IgA IgD | %IgAggregates | ||
| PatientNormal ± SD | 82.480±4 | 3.98±4 | 10.4 4.9 5.5 10±4 2± 1 8±3 | 12.8 18 ±7 |
Table 2—Responses to Mitogens in Patient and Healthy Matched Control
| Mitogen | Patient | Control |
| — | 113 ±5 | 370 ±17 |
| Con A 5|ig/ml | 9,576 ±267 | 27,282 ±925 |
| Con A 1 tLg/ml | 951 ±83 | 4,183 ±679 |
| PHA 20|xg/ml | 24,869 ±543 | 34,362 ±418 |
| PWM 5|ig/ml | 9,848 ±363 | 16,070 ±2600 |
| PWM 1 jig/ml | 6,505 ±854 | 18,788 ±5109 |